Optical medical device
Medical imaging clinical standards (MRI, nuclear medicine, CT…) face limitations in operative room and point of care conditions, due to technical, cost and regulatory (ionizing radiation…) constraints. Optical medical devices are relevant in theses contexts because they are easy to handle, reliable, generally low-cost, allow high rate acquisition, and have also the advantage to be non-contact imaging modalities. This research axis tackles the relevance of new optical imaging approaches for:
- (i) point of care and bedside non-invasive monitoring of the cerebral metabolism and brain pathologies;
- (ii) interventional and intraoperative imaging during neurosurgery of brain pathologies, and in particular for brain cancer.
These works involve developments in instrumentation (Fluorescence, hyperspectral and time-resolved optical imaging), real-time information processing and biomarker quantification methods driven by the clinical application and ANSM validated prototype for clinical trials.
Point of care brain imaging:
We have developed a point of care broadband time-resolved multi-channel near infrared spectroscopy system that can monitor non-invasively the physiological responses of the adult human brain. In-vivo experiments on healthy volunteers were performed to monitor the hemodynamic response in the brain during a cognitive task. Moreover, looking at the response at different time windows, we could monitor the hemodynamic response in depth, enhancing the robustness of detection of the cortical activation. Those first results demonstrate the ability of our system to discriminate between the responses of superficial and deep tissues, addressing an important issue in fNIRS [Lange-2018 Applied Optics].

Fig. Example of responses for subject 4, for every window (early window, late window, and CW-like window), and for every optode. The red thick line represents the [HbO2] concentration changes and the blue thin line represents the [HHb] concentration changes. The shadow regions represent the standard error of the mean. The picture shows the positioning of every optode (S is the source)
Intraoperative imaging for neurosurgery guidance:
The resection of gliomas during surgery is a procedure which is always a trade-off between the resection of a maximum amount of tumor cells and the preservation of functional areas. The intraoperative identification of brain functional areas is tackled by considering the neurovascular coupling which induces variations of local tissue perfusion and oximetry when brain cortical areas are activated.
Hyperspectral optical imaging is used to measure the brain hemodynamics triggered by physiological stimuli. In collaboration with Team MYRIAD [M. Sdika et al-2019-. MedIA, 2019] a fast real-time algorithm was developed and applied, yielding motion-corrected RGB videos of brain during neurosurgery. A quantification model [Caredda-2019- et al. Neurophotonics] taking into account the brain heterogeneity in the physical model of biomarkers then produced quantitative maps of functionality biomarkers.

Figure : Identification of the position of the motor cortex during neurosurgery with optical video. The letters M indicate motor areas and S indicate sensitivity areas (determined with gold standard electrical stimulation). The added false color scale indicates a proposed biomarker after appropriate thresholding and linked to oxy- and deoxy-hemoglobin parameters.
Concerning tumor localization, the gold standard is still an anatomopathological procedure and is thus time-consuming. An alternative approach could be intraoperative 5-ALA Protoporphyrin IX (PpIX) fluorescence imaging but as carried out now, it still lacks sensitivity. In a previous work, [B. Montcel et al. Biomed Optics Express 2013] it was shown that the PpIX fluorescence spectrum displays a spectral complexity which is relevant for tumor margin identification. Further in vitro, ex vivo and in vivo studies strongly hints that there exists two close emission spectra of PpIX that are indeed relevant; one peaking at 620 nm and the other at 634 nm [L. Alston-2018- et al. J. Biomed. Optics, 2018]. We developed an intraoperative prototype validated by the ANSM and led a clinical trial (NCT02473380 https://clinicaltrials.gov) on 10 patients resulting in the definition of new biomarkers of PpIX fluorescence emission. These works were led in close collaboration with Jacques Guyotat (Neurosrugery service HCL) and Mathieu Hebert (Lab. Hubert Curien). These results [L. Alston- et al. 2019-Biomed. Optics Express], 2019; [P. Leclerc-2019- et al., Scientific Reports] suggest that these biomarkers could increase the sensitivity of the 5-ALA induced PpIX fluorescence technique in low-density margins and improve the definition of the boundary between tumor margin and healthy tissues in high and low-grade gliomas.

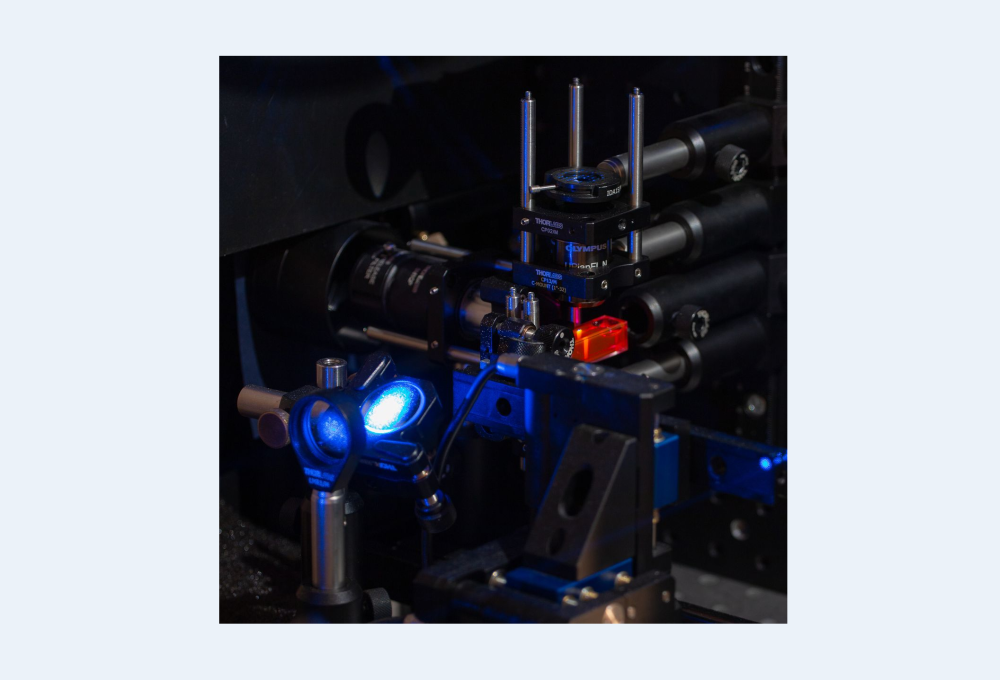
Figure : Intraoperative system developed at CREATIS and used in a clinical study on 10 patients; Data analysis of the results with unsupervised classification in a T-SNE reduced space. K-means classification and GMM classification both with 4 clusters.
Endoluminal MR/Optics:
In France, colorectal cancer is the second cause of cancer death. Endoluminal coil are able to achieve significantly higher local SNR than conventional external surface coil allowing wall assessment of colon. Tissue characterization based on Mr imaging and spectroscopy can be further improved with conventional and confocal optic endoscopy as demonstrated in vivo on a mouse model of colitis during two longitudinal follow-up.

Colorectal tissue lesion characterization based on MR imaging and spectroscopy with conventional and confocal endoscopy.
Although the local high sensitivity of endoluminal coils allows to achieve the required spatial resolution of MR images for analysis of colon wall, such inner coils involves risks for the patient. Indeed, the local SAR induced by the radiofrequency electric field, due to the presence of the cable connecting the coil with the imaging system, can cause local heating that need to be overcome. In this context, our research follow two objectives: (i) to perform an electro-optical conversion of the radiofrequency MR signal to remove the patient's safety issues by replacing the galvanic cable with optical fiber; (2) To characterize and validate electric field probes designed by our partner KAPTEOS to monitor in real time the local SAR and to measure electric field distribution created by manufactured MR coils.
MEMS:
Micro Electro Mechanical Switches (MEMS) compatible with MR was introduced by GE Healthcare few years ago. In the literature, MEMS were successfully used as switches: i) to achieve active decoupling; ii) to open or close portions of metallic conductors to modify coil loop geometries; iii) to shift the resonance frequency of coil loop in the case of dual tuned RF coils. In this context, our goal is to investigate the benefit of MEMS for endoluminal coil MR imaging. Indeed, endoluminal coils introduced in the colon and bowel, although achieving high local SNR allowing wall analysis, suffer from sensitivity-map variations as a function of coil-orientation with respect to B0. Reconfiguration of loop coil geometries using MEMS is able to resist the adverse effects of orientations to B0.

Scheme of orientation regarding to B0 during endoluminal coil navigation
Sono-cardioprotection project
The importance of myocardial infarction and its consequences in terms of heart failure and cardiovascular mortality make it a major public health problem in developed countries. The size of the infarction is the major factor in the prognosis after acute myocardial infarction (AMI). Interventions to reduce the final size of the infarction are therefore of major clinical interest to improve the prognosis of patients managed for myocardial infarction. The current management of myocardial infarction aims to reinfuse the myocardium as soon as possible, by primary percutaneous coronary angioplasty as often as possible. However, experimental and clinical studies have shown that sudden reperfusion also has deleterious effects on ischemic myocardium and induces additional reperfusion lesions. This damage after reperfusion can contribute up to 40% of the final size of the infarction.
In this context, our group has been working for many years to 1) propose new imaging methods to explore the impact of myocardial infarction on the heart, 2) understand the variability of measurements and results according to the time required to treat it, 3) recommend a post-infarction exploration chronology and optimized imaging protocols, 4) validate new imaging exploration methods dedicated to the specific study of inflammation. Indeed, we need to understand how the inflammatory state of the heart, at the time of therapy, can influence the therapeutic results themselves.
The TSONOAMI project builds on this precedence and aims to propose a new method of protection based on "mechanotransduction" (MT) and ultrasonic waves to help reperfusion after an AMI. TM effects can be achieved by applying low-energy ultrasound waves to the damaged area, which may have a micro-massage effect on the capillaries, help restore vascularization and restore normal heart function.
The validation of this innovative treatment method will be carried out on an experimental model of a large animal (pig). This step is essential before any subsequent implementation on patients with AMI can be considered. The physicians involved in this study have extensive experience in the field of cardiac protection after an AMI, which would facilitate the rapid transfer of this treatment to the clinic in the event of success with high impact public health outcomes.